Abstract
Background:
The depth of response both pre- and post- autologous stem cell transplant (ASCT) has been shown to correlate with clinical outcome for myeloma patients. Maximizing response can be achieved by modifying therapy either at induction, transplant, consolidation or during maintenance. In this work we explore the role of pre-transplant induction therapy in the UK NCRI Myeloma XI clinical trial and whether the number of cycles of induction impacts on clinical outcome.
Methods:
Myeloma XI recruited 2568 newly diagnosed transplant eligible patients. Patients were initially randomized between immunomodulatory agent containing triplets comprising cyclophosphamide, dexamethasone and either lenalidomide or thalidomide (CRD vs CTD). Patients were treated to maximum response and for a minimum of four cycles of therapy. At maximum response, patients with a VGPR or CR proceeded straight to ASCT, whilst those with a suboptimal response (PR/MR) entered a second randomization between a bortezomib containing triplet (CVD) or no further therapy, and those with refractory disease (SD/PD) all received CVD. The protocol was amended subsequently to compare the upfront quadruplet KCRD to the response adapted approach. After ASCT patients were randomized between maintenance therapy with lenalidomide +/- vorinostat or no further therapy.
In this exploratory analysis we compared baseline characteristics and outcomes for patients who received 4 cycles of initial induction (the protocol defined minimum), 5-6 cycles or >6 cycles. Patients who received <4 cycles were excluded.
Results
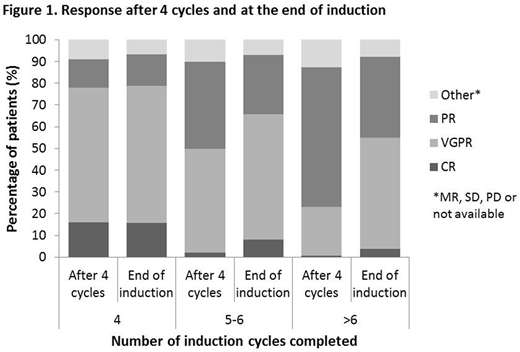
In total 787 patients completed 4 cycles of initial induction, 1223 had 5-6 cycles and 281 had >6 cycles. A comparison of baseline characteristics showed that the group receiving more induction therapy was associated with a higher ISS stage and greater disease burden at baseline. The percentage of patients with ISS stage II/III was greater in those receiving more cycles of therapy, 4 cycles 57.6%, 5-6 cycles 62.2%, >6 cycles 67.3%. The percentage bone marrow infiltration increased (BM plasma cells >20% was 32.3%, 42.3% and 43.4% respectively). Patients with an IgG paraprotein made up a larger proportion of those receiving more cycles 50.2%, 65.1% and 67.3% respectively, whereas those with IgA or light chain disease showed the opposite pattern. Age, sex and performance status showed no association. Cytogenetic risk was equally distributed across groups with a subset of standard risk patients requiring additional cycles of therapy, indicating some slow responders even in this good prognosis group. KCRD had a superior time to and depth of response; patients receiving KCRD required a median of only 4 cycles and had a much higher proportion of patients receiving only 4 cycles (KCRD 49.8%, CRD 29.7%, CTD 21.7%).
Response at the end of 4 cycles of therapy and at the end of initial induction, Figure 1, shows that additional cycles deepened response. This was consistent across all induction regimens. Patients receiving >4 cycles of therapy, however, never attained as deep responses as those whose maximum response was achieved by 4 cycles and were therefore also more likely to receive subsequent therapy with CVD intensification in the response adapted arm of the study.
Overall, the depth of response at the end of initial induction was associated with a significant effect on PFS (Median PFS: CR 63.3 months, VGPR 43.8 months, PR 30.6 months, p<0.0001) with a trend toward the same effect on OS. There was no statistically significant difference in progression-free or overall survival for patients receiving 4, 5-6 or >6 cycles of initial induction.
Conclusions:
The results suggest that continuing induction to maximum response is not detrimental to patient outcome and may have overcome an adverse impact of a less deep response. Continuing induction therapy until maximum response may improve outcomes for patients with an otherwise suboptimal response at the end of 4 cycles.
Pawlyn:Amgen: Consultancy, Honoraria, Other: Travel Support; Janssen: Honoraria, Other: Travel support; Celgene Corporation: Consultancy, Honoraria, Other: Travel support; Takeda Oncology: Consultancy, Other: Travel support. Jackson:Merck Sharp and Dohme: Consultancy, Honoraria, Speakers Bureau; Amgen: Consultancy, Honoraria, Speakers Bureau; Roche: Consultancy, Honoraria, Speakers Bureau; Takeda: Consultancy, Honoraria, Other: Travel Support, Research Funding, Speakers Bureau; Celgene: Consultancy, Honoraria, Other: Travel Support, Research Funding, Speakers Bureau. Cairns:Merck Sharp and Dohme: Research Funding; Amgen: Research Funding; Celgene: Research Funding. Striha:Celgene: Research Funding; Janssen: Research Funding; Amgen: Research Funding; Abbvie: Research Funding; MSD: Research Funding. Hockaday:MSD: Research Funding; Janssen: Research Funding; Amgen: Research Funding; Millenium: Research Funding; Celgene: Research Funding; Abbvie: Research Funding. Jones:Celgene: Honoraria, Other: Travel support, Research Funding. Boyd:Celgene: Consultancy, Honoraria, Other: Advisory role; Janssen: Honoraria, Other: Travel and Accommodation expenses; Novartis: Consultancy, Honoraria. Kishore:Celgene: Honoraria; Takeda: Honoraria, Other: travel support. Garg:Takeda: Other: Travel Grant; Amgen: Honoraria, Other: Travel Support; Novartis: Other: travel support, Research Funding; Janssen: Honoraria. Williams:Celgene: Honoraria, Other: travel support, Speakers Bureau; Amgen: Honoraria, Speakers Bureau; Takeda: Honoraria, Other: travel support, Speakers Bureau; Novartis: Honoraria; Janssen: Honoraria, Other: travel support, Speakers Bureau. Karunanithi:Celgene: Other: Travel support, Research Funding; Janssen: Other: Travel support, Research Funding. Lindsay:Janssen: Consultancy; Novartis: Other: Travel support; Celgene: Honoraria, Other: Travel support; BMS: Consultancy, Other: Travel support; Takeda: Other: Travel support. Jenner:Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Cook:Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Amgen: Consultancy, Honoraria, Research Funding, Speakers Bureau; Seattle Genetics: Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Research Funding, Speakers Bureau; Celgene Corporation: Consultancy, Honoraria, Research Funding, Speakers Bureau; Glycomimetics: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Speakers Bureau; Janssen: Consultancy, Honoraria, Research Funding, Speakers Bureau. Russell:Jazz Pharma: Speakers Bureau; Pfizer: Consultancy, Honoraria, Speakers Bureau; Daiichi Sankyo: Consultancy. Kaiser:Bristol-Myers Squibb: Consultancy, Other: travel support; Chugai: Consultancy; Janssen: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Takeda: Consultancy, Other: travel support; Celgene: Consultancy, Honoraria, Research Funding. Drayson:Abingdon Health: Equity Ownership, Membership on an entity's Board of Directors or advisory committees. Owen:Janssen: Consultancy, Other: Travel support; Celgene: Consultancy, Honoraria, Research Funding; Takeda: Honoraria, Other: Travel Support. Gregory:Celgene: Consultancy, Honoraria, Research Funding; Merck Sharp and Dohme: Research Funding; Janssen: Honoraria; Amgen: Research Funding. Morgan:Takeda: Consultancy, Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria; Janssen: Research Funding; Celgene: Consultancy, Honoraria, Research Funding. Davies:Amgen: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal